Common pharmaceutical approvals for better public health
Counterfeit medicines, substandards, a still poorly regulated pharmaceutical sector… In the six member countries of the Economic and Monetary Community of Central Africa (CEMAC ), the quality of medicines in circulation is a vital issue. To support the growth of the pharmaceutical sector in these countries, L’Initiative conducted a technical assistance mission with the Coordination Organization for the Fight against Endemic Diseases in Central Africa (OCEAC ), between May 2020 and May 2021. Maxime Desmaris, pharmacist and Health Project Manager at Expertise France, looks back on this major public health challenge.
Why is it necessary to strengthen drug approval?
Approval consists, among other things, of validating the data provided by the laboratory that is applying for marketing authorization for one of its products so that it can be marketed. This means studying the file, carrying out various visits to the production or distribution sites and analyzing the medicines. Only then can the public be guaranteed that a medicine is of good quality and meets certain standards.
Although many drugs now enter CEMAC countries through development programs – and therefore already meet international standards – their number is limited. These countries need their own approval system to ensure a good supply of drugs that treat pathologies neglected by donors, such as non-communicable diseases such as cardiovascular diseases, respiratory diseases or diabetes.
What are the consequences of a failing drug approval system ?
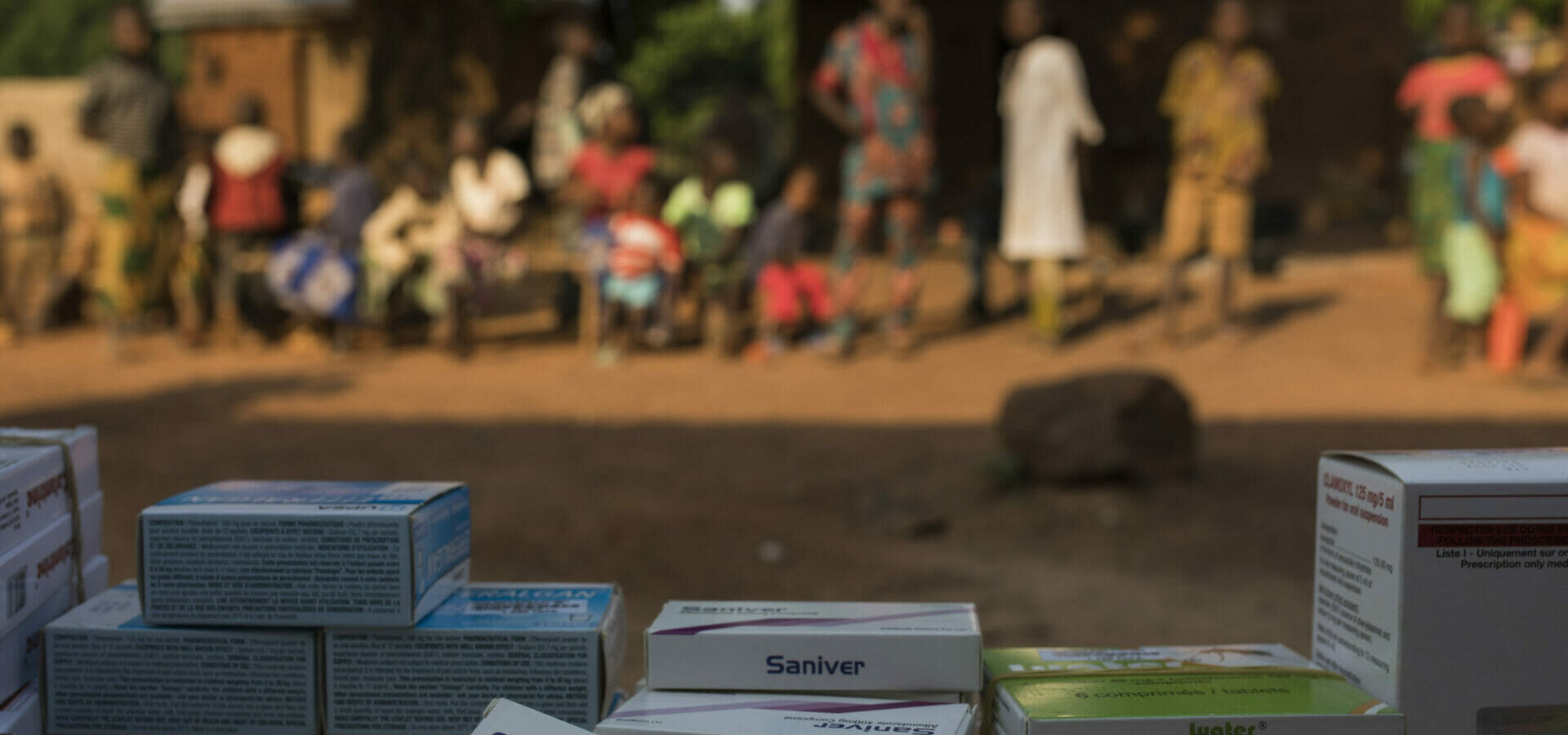
One in ten drugs sold worldwide is either falsified or substandard, and in some African countries this figure can reach up to seven in ten drugs according to WHO estimates. Without a coherent and effective approval system, populations are quickly confronted with falsified or substandard drugs. At best, these drugs do not have the expected efficacy. At worst, patients who think they are treating themselves will in fact develop side effects, or not treat their pathology and therefore perhaps die from it. Falsified or substandard drugs against malaria and tuberculosis are alone responsible for several hundred thousand deaths per year worldwide.
This phenomenon is particularly serious in Central Africa. It is directly linked to the lack of resources of States or of the various public bodies responsible for these approvals. As a result, for years, parallel distribution channels for falsified or substandard medicines have been well established.
How will the proposal of the L’Initiative support mission help improve the situation?
The regional system of pooling practices, human and financial resources that we propose to CEMAC countries makes it possible to create a coherent and common approval for all medicines in this Central African region. File reviews can thus be carried out jointly – which makes it possible to share costs, resources and expertise – or produced by one of the countries in compliance with a shared regulatory framework. The medicine then benefits from a simplified procedure to access the market of other countries. This is exactly what is done in Europe where the marketing authorisations for a medicine go either through the European authorities, which validate the medicine for all EU Member States, or through the authorities of one country – the others can facilitate the procedure on their market.
We have also created a database and an online platform that allows information to be shared between the authorities of the six countries. The public will also be able to consult part of this data to check whether their medicine has been approved in their country.
How can we ensure the sustainability of the proposed new system?
It is important to ensure that these joint reviews do not represent a significant financial burden for these countries. Approving a drug is expensive in terms of travel, analysis, human time, and management of IT tools. By transferring these costs to the laboratories that apply for marketing authorization, the study of the approval file can be carried out without additional cost to public services. This is what is done in other countries such as France. However, one limit to this is the laboratory’s desire to register its drug.
States must now absorb this methodology, take ownership of it and adopt these good practices. The report of the three experts in charge of this mission formulated clear and precise recommendations and was translated into the official languages of the six member countries. It will be presented at an upcoming meeting of CEMAC Ministers of Health. The rest depends on the decision-makers who, we hope, will show the will to strengthen their health product management system.