Operational research: improving access to HPV screening and vaccination
On 17 November, World Cervical Cancer Elimination Day reminds us of the scale of a burden that remains significant: around 660,000 new cases and 350,000 deaths were estimated in 2022, more than 90% of which occurred in low- and middle-income countries. Cervical cancer remains one of the few non-communicable diseases for which an elimination strategy is considered achievable, provided that countries can ensure effective access to human papillomavirus (HPV) vaccination, HPV screening, triage (the step that makes it possible to identify, among HPV-positive women, those at increased risk of precancerous lesions), and treatment.
Producing evidence to transform health policies
The global “90-70-90” strategy adopted by WHO in 2020 sets three targets to be reached by 2030:
- 90% of girls vaccinated against HPV before the age of 15;
- 70% of women screened at ages 35 and 45 with a high-performance HPV test;
- 90% of women presenting precancerous or cancerous lesions having access to treatment.
But in many countries, progress towards these targets is hindered by persistent operational constraints: limited laboratory capacities, irregular organisation of sample transport, heterogeneity of triage models, variable availability of treatment, and loss to follow-up after a positive test. Added to this are obstacles linked to the gradual integration of HPV screening into national guidelines and to the still uneven mastery of techniques within services. To help address these constraints, L’Initiative has been funding since 2023 three operational research projects in Cameroon and Ghana, led by French and local research laboratories and committed national institutions. Their objective: to produce contextualised evidence to adapt national strategies to field realities.
C3UC3 (Cameroon): observing the pathway from women’s perspective
C3UC3, conducted by the Institut Bouisson Bertrand, analyses the real conditions of access to HPV screening in health facilities in Yaoundé and its outskirts. The project shows that women’s entry into the pathway depends not only on the availability of the test but on a set of social, economic, and relational factors: perception of risk, ability to project themselves into a pathway with multiple steps, mobility, trust in services, the role of community workers, and exposure to gender-based violence.
In this urban context that nevertheless has infrastructure, self-sampling, which is generally well accepted, is not enough to lift obstacles when information is unclear or when care appears difficult to understand. C3UC3 highlights the importance of intermediation work—counselling, support, translation of technical messages—to turn an operational screening offer into a service that is genuinely used, particularly by women living with HIV, whose risk of developing cervical cancer is significantly higher.
The video below shows, through testimonies from women, community health workers and healthcare professionals, why combining clinical approaches with community engagement is essential to improve access to HPV screening and care in Cameroon.
OPTI-TRI (Cameroon): documenting gaps at the triage stage
OPTI-TRI, led by the Institut de recherche pour le développement (IRD), focuses on the most critical stage of the pathway: the management of HPV-positive women. Unlike C3UC3, the project is implemented in rural and peri-urban areas, where constraints related to distance, human resources, and clinical supervision strongly shape the feasibility of triage.
The study compares centralized, decentralized, and hybrid configurations and analyses their viability across different territories. Early data show that centralized models generate significant loss to follow-up due to distance and delays, while decentralized models improve access but require sustained clinical supervision to ensure quality of examinations. OPTI-TRI highlights the variability of colposcopy between platforms, the challenges of standardization, and the potential contribution of decision-support tools, including image analysis, to secure clinical interpretation. Far from imposing a single model, the project specifies the concrete conditions that allow each configuration to function sustainably.
Ghana: integrating HPV screening into HIV services
In Ghana, the operational research conducted by the Noguchi Memorial Institute for Medical Research addresses a major blind spot: despite a risk up to six times higher of developing precancerous lesions, women living with HIV do not yet benefit from systematic HPV screening in ART Clinics. The gap between international standards, where screening is part of routine care, and local practices justifies in-depth fieldwork.
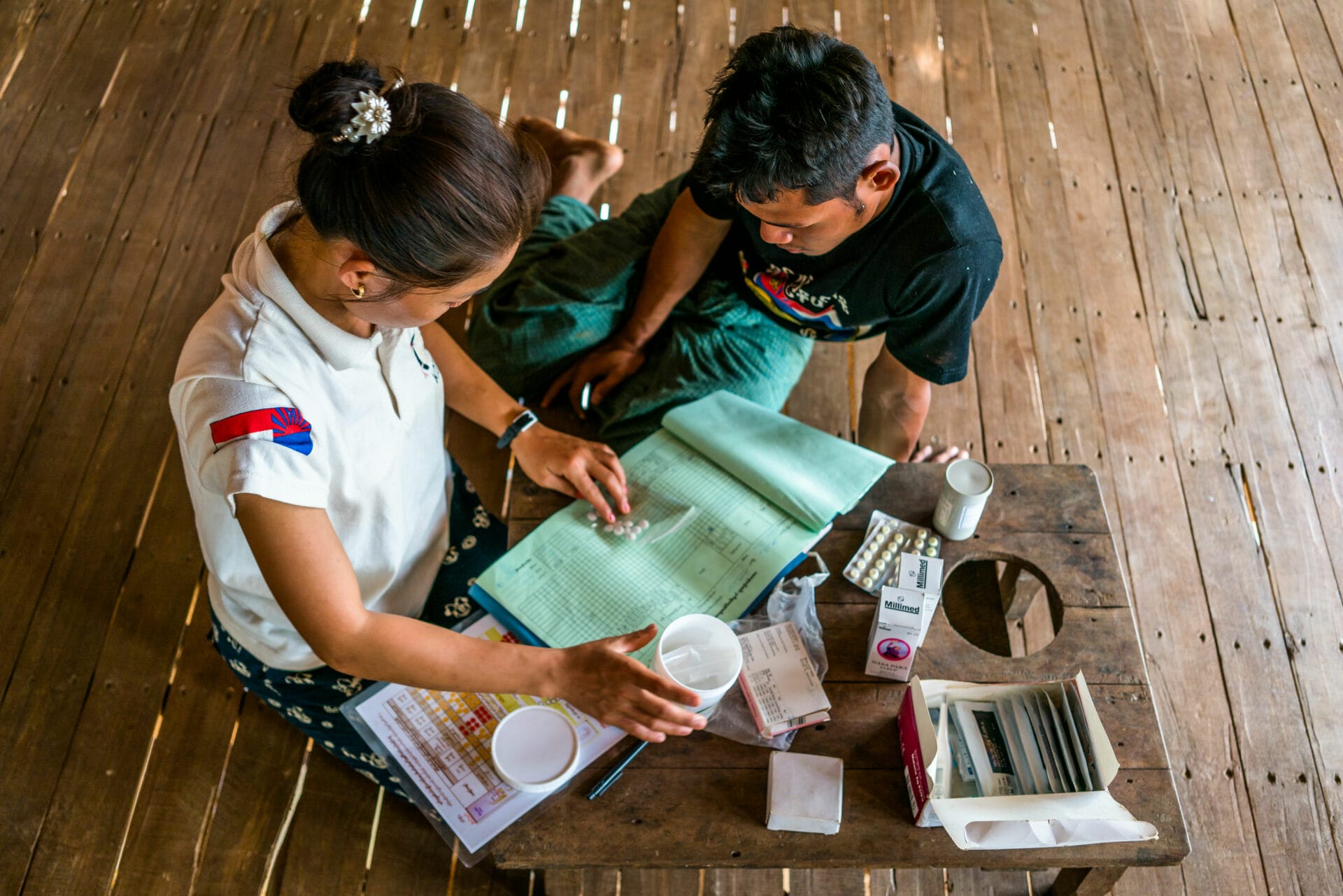
The project examines the feasibility of an integrated model tested in several facilities in the Greater Accra, Central, and Eastern regions. It analyses how to organise, within HIV services themselves, a complete pathway: information, sampling, HPV PCR analysis (including through existing GeneXpert platforms), interpretation of results, and referral for triage. This integration also requires training nurses in screening and lesion identification, in a context where workload and logistics must be rebalanced.
Initial findings show that a “one-stop” model significantly reduces loss to follow-up and strengthens continuity of the pathway, provided that protocols are harmonised and minimal clinical supervision is ensured. The project also produces structuring documentation (procedures, guides, protocols) intended to support the development of a future national model for integrating HPV screening into HIV services.


Informing programmatic decisions
By focusing the analysis directly on women’s pathways, the actual workload of teams, and the concrete functioning of facilities, the three projects provide a detailed and complementary understanding of how HPV screening operates. They shed light on the actual delays between testing and triage, the organisation of services, the feasibility of centralized or decentralized configurations, the conditions for coherent follow-up for women living with HIV, and the minimum requirements to ensure triage quality.
This data enables health authorities to revise their strategies realistically: sizing of laboratories, organisation of workflows, prioritisation of districts, choice of triage modalities, and adjustment of clinical supervision. By documenting the gaps between theoretical models and real-world functioning, operational research reduces uncertainty and secures programmatic decision-making.
Evidence as a tool for national steering
Operational research today occupies a central place in the response to cervical cancer. It makes it possible to move beyond theoretical models or normative recommendations to better understand how women actually navigate the system, how teams handle the increasing volume of screening, and which configurations are viable and relevant in constrained environments.
By producing robust data grounded in local contexts, operational research offers decision-makers a solid framework to adapt national policies and secure continuity of the screening–triage–treatment pathway. It is this capacity to clarify feasibility conditions, test realistic configurations, and guide the adjustment of national policies that makes operational research an essential lever for progress towards cervical cancer elimination.