To fight drug-resistant tuberculosis: efficient laboratories and accessible treatments
Tuberculosis treatment resistance complicates the fight against the disease. In response, The Initiative focuses on healthcare human resources and capacity building. Explanations on the 2024 World Tuberculosis Day.
Tuberculosis remains one of the deadliest diseases in the world: it killed more than 13 million people in 2022, mainly due to inequitable access to diagnosis and care. About 106 million people contract tuberculosis each year, and nearly half are not diagnosed and thus do not have access to medication. Yet, effective treatments exist that can cure most infections within 4 to 6 months.
The lack of diagnosis is not the only difficulty that could jeopardize the global goal of eradicating the pandemic by 2030. Antibiotic resistance also represents a major obstacle towards a tuberculosis-free world
Forms of tuberculosis resistance
Resistance occurs when antituberculosis drugs are not properly prescribed (using a single drug rather than a combination of antibiotics, or using poor quality or poorly stored drugs) or when patients prematurely interrupt treatment.
Multidrug-resistant tuberculosis occurs when patients do not respond to isoniazid or rifampicin, the two most effective first-line antituberculosis drugs. In some cases, broader resistance can develop. This is referred to as multidrug-resistant tuberculosis (MDR-TB: cross-resistance to isoniazid and rifampicin) or extensively drug-resistant tuberculosis (XDR-TB: resistance to isoniazid, rifampicin, and other second-line drugs). To limit the development of these resistances, access to more expensive (and thus less available) drugs with often more toxic side effects is necessary. In the most severe forms, drug resistance often leaves patients without any therapeutic option, condemning them.

Only two out of five people had access to treatment
in 2022, among patients with drug-resistant tuberculosis. Like drug-susceptible tuberculosis, multidrug-resistant tuberculosis can be transmitted, especially in crowded places, such as prisons or hospitals : it represents a threat to health security.
Tuberculosis: the voices of research
Gisèle Badoum Ouedraogo, expert in epidemiological dynamics and pulmonologist in Burkina Faso, discusses the development of antibiotic resistance as well as the innovations brought by operational research to fight it.

Strengthening the human and technical skills of health infrastructures
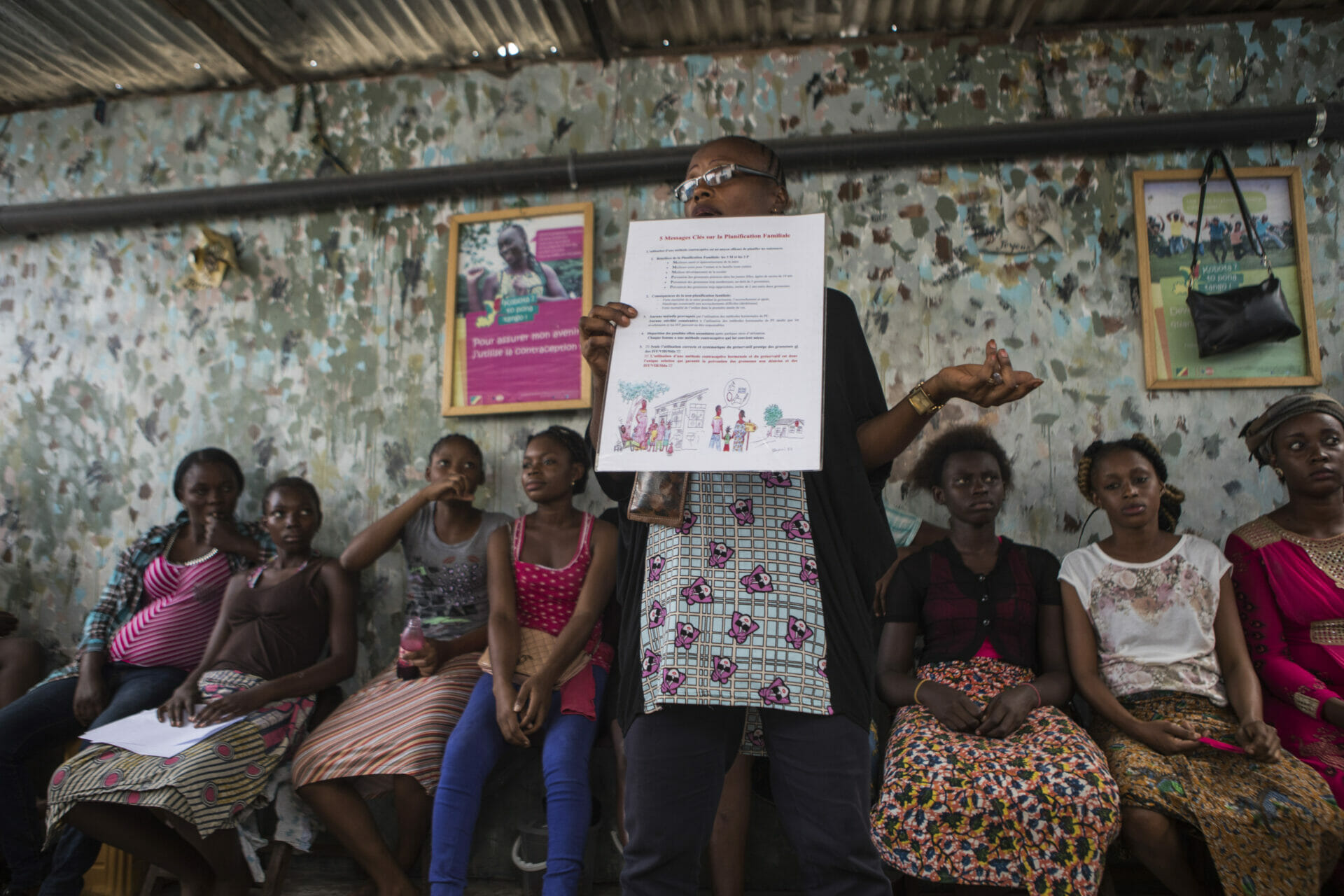
In order to detect resistances and choose the most suitable therapeutic options, efficient reference laboratories and well-trained staff are crucial. The surveillance role of national reference laboratories (NRL) is a fundamental element of the fight against tuberculosis. They must be able to receive highly infectious samples while preserving the health of personnel and the environment and to identify resistances circulating in the country. These resource and skill challenges for healthcare human resources are one of L’Initiative’s strategic priorities.


Under the supervision of health personnel including the head nurse of Biyem-Assi hospital, children are screened for tuberculosis by sputum sampling (Yaoundé – Cameroon)
Towards more accessible and effective treatments
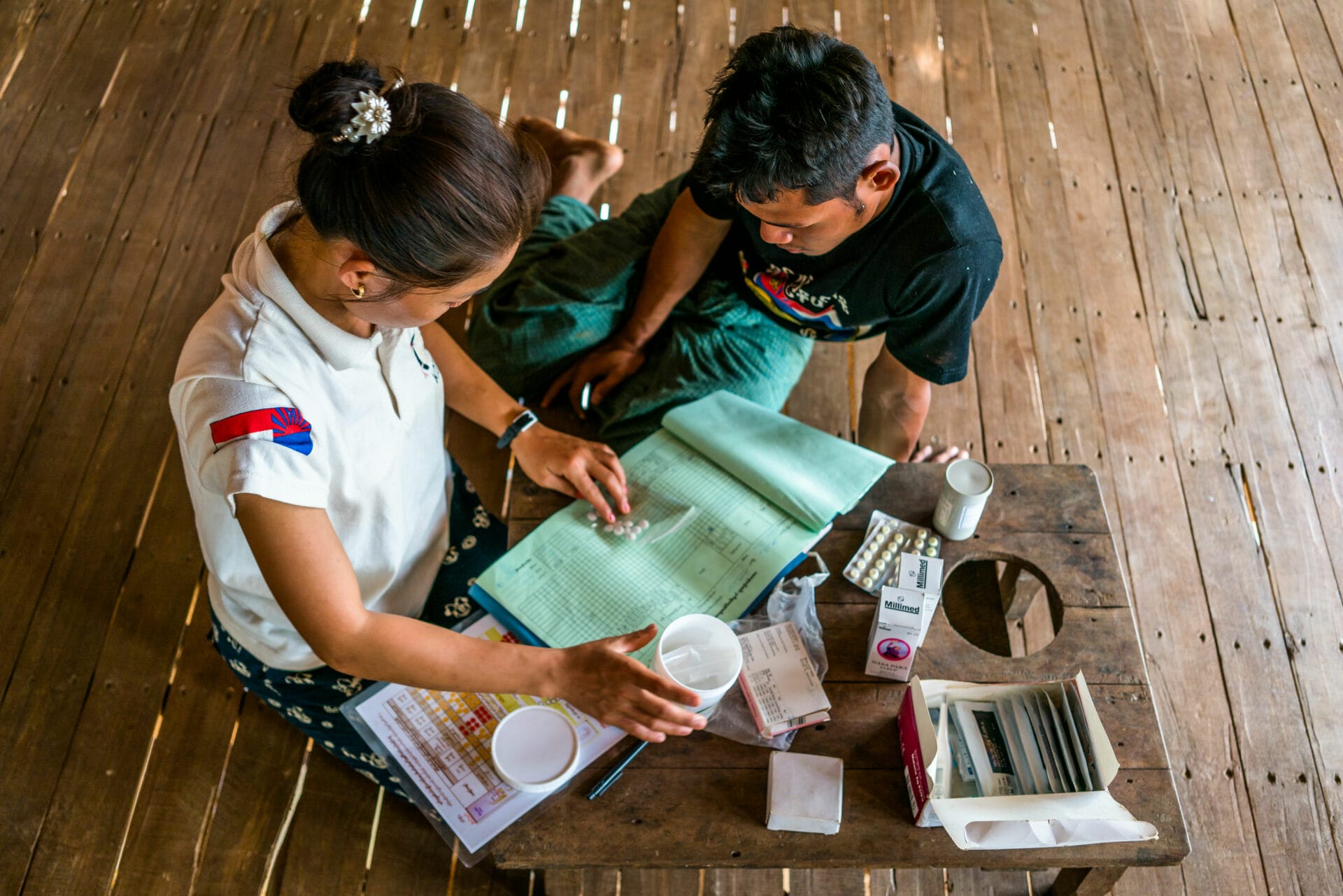
Compliance to treatments is one of the conditions to prevent the emergence of mutations and resistances. However, the patient-perceived treatment burden can lead to interruption of care. Nausea and vomiting, damage to peripheral nerves causing numbness or pain, gastrointestinal problems, or eczematous reactions: the side effects of tuberculosis treatment are severe and can affect the quality of life of patients. Added to this is the discouraging duration of treatments for drug-resistant tuberculosis (about one year), which leads some patients to prematurely interrupt their follow-up, compromising their recovery and fueling resistances. When exposed to low doses of drugs, bacteria do not succumb but adapt.
To improve treatment compliance, significant progress has been made in recent years, in particular with the development of shorter and less aggressive treatment protocols that should promote better compliance and thus prevent resistances.


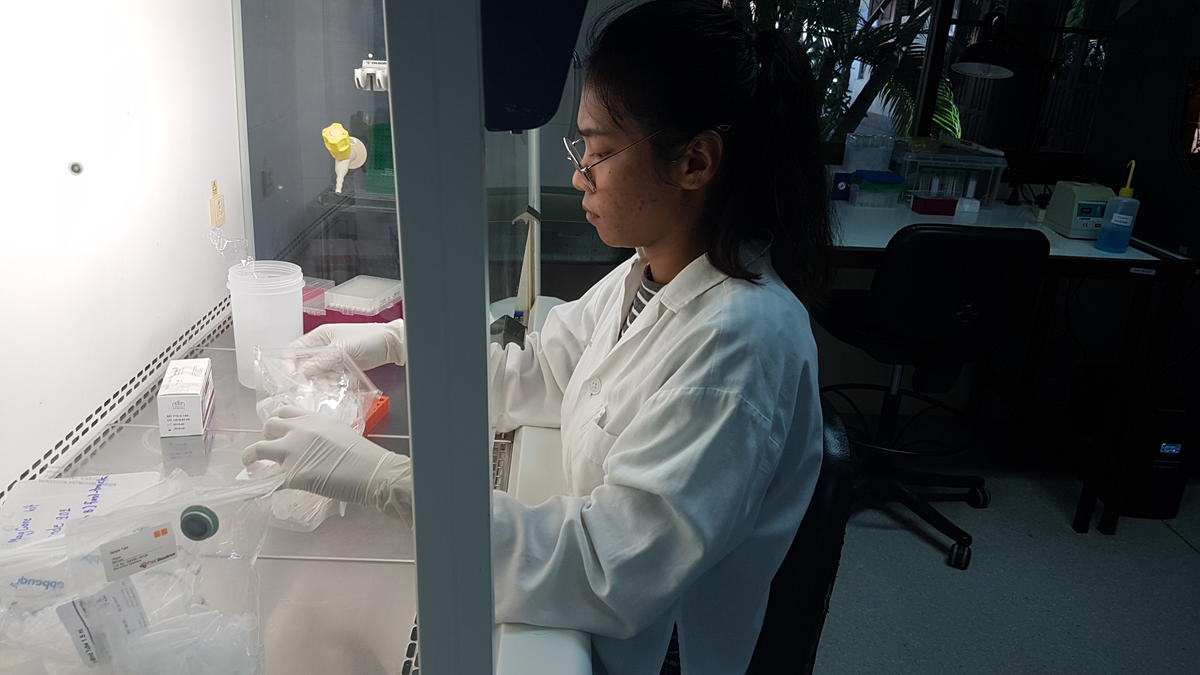
Hospital staff prepare to test tuberculosis samples for resistance
Another significant advancement is the end of the bedaquiline patent, a result of advocacy supported by organizations like Médecins sans Frontières (Doctors Without Borders), paving the way for lower-cost distribution of this vital molecule. Bedaquiline, included in all therapeutic schemes recommended by the World Health Organization, is expected to revolutionize the management of resistant forms of tuberculosis, offering a new, less burdensome, and cheaper therapeutic option for caregivers and patients.