AHRI-APOPO: Targeting, Screening, and Treating Tuberculosis in Disadvantaged Communities in Addis Ababa
Ethiopia is among the 30 countries most affected by tuberculosis and HIV/tuberculosis co-infection. According to the World Health Organization (WHO), 188,000 people were infected in the country in 2023. Strongly associated with poverty, the prevalence of this disease has worsened due to COVID-19, internal conflicts, and the global economic situation. The disadvantaged populations of Addis Ababa, Ethiopia’s capital, are among the most affected in the country, making tuberculosis a major public health issue. Negussie Beyene and Aline Serin share insights into the AHRI-APOPO project, supported by L’Initiative, and its goals of innovative screening and awareness-raising.
What is the situation in Addis Ababa?
Negussie Beyene: Addis Ababa is an overcrowded city experiencing a constant influx of people due to internal conflicts or migration in search of better living conditions. While official figures estimate the population at five million, unofficial assessments suggest it could be between 10 and 15 million, as many new arrivals are not registered. This high population density, particularly in peripheral areas, creates ideal conditions for the spread of tuberculosis.
Aline Serin: Indeed, the Ethiopian capital is undergoing a late but rapid urban transition. Urban development projects, such as those under the Corridor Project, were intended to modernize the city but have led to the eviction of many residents. Without adequate relocation solutions, these people are forced into overcrowded suburban areas, further accelerating the spread of the disease.
Can you explain the community-based approach adopted by the project to fight tuberculosis?
Aline Serin: The major challenge in the fight against tuberculosis in Ethiopia lies in education and awareness. The population is often poorly informed about the disease and unaware that free screening and treatment services are available. The distance to health centers is another significant barrier, leading many Ethiopians to delay seeking medical attention until their condition becomes severe. It’s a complex decision, but for many, traveling to a distant health facility can seem less urgent compared to other immediate needs.
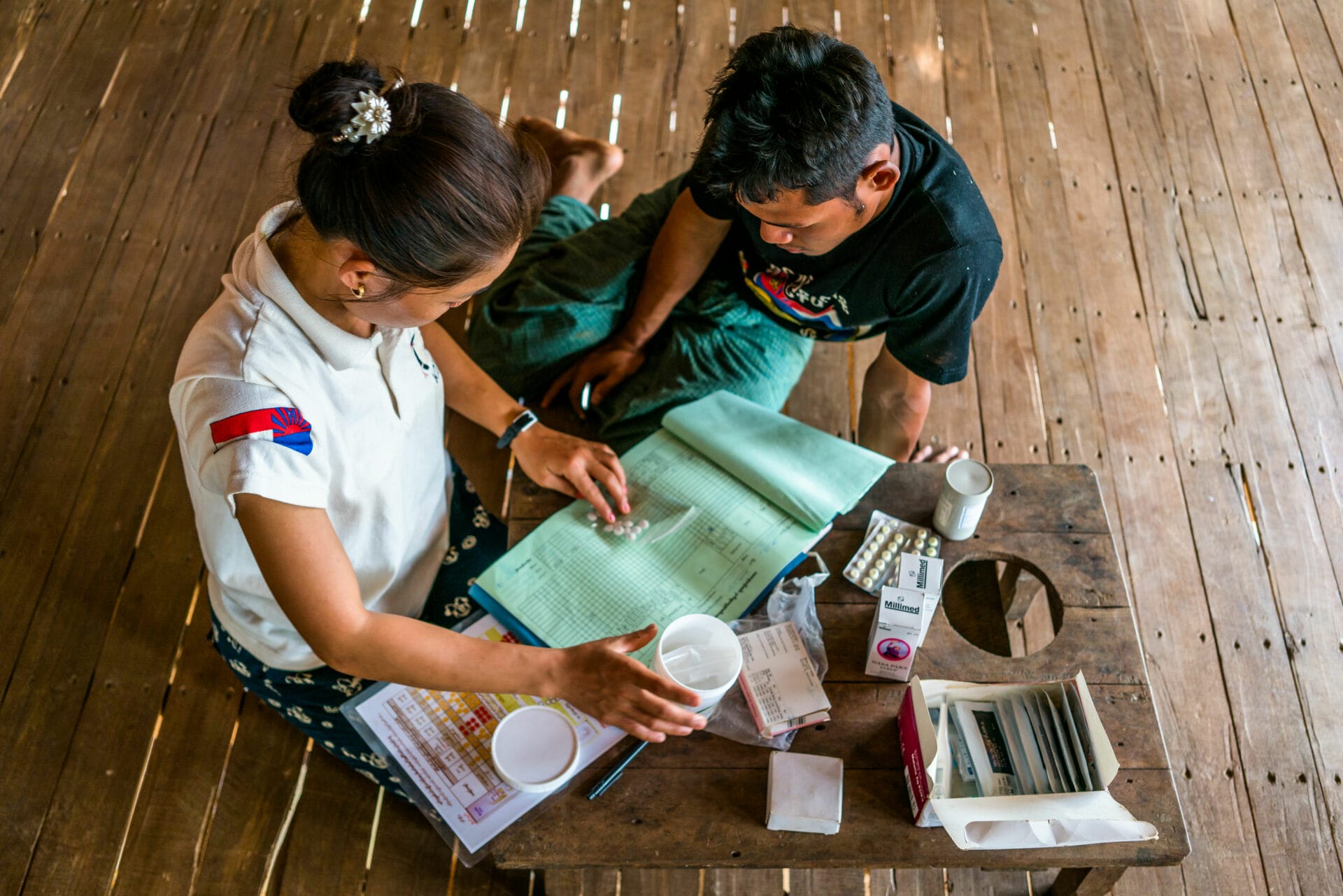
Negussie Beyene: Despite the existence of around a hundred health centers in the city, the most vulnerable populations—migrants, people struggling with alcoholism, or those living on the streets—often lack knowledge about their rights and access to free healthcare services. In response, the AHRI–APOPO project works with local civil society organizations to reach those most excluded from the healthcare system. We have set up a team of professionals, including urban health workers, specifically trained to raise awareness and intervene directly within communities. Their role is to educate people about tuberculosis, its modes of transmission, key symptoms, available screening and treatment methods, and the risks of not seeking care. Through these information sessions, community members become better informed and, in turn, help us identify symptomatic individuals within their neighborhoods. Once potential cases are identified, we collect sputum samples for free tuberculosis screening. If the test confirms tuberculosis, our health workers accompany patients to healthcare centers to ensure they start treatment immediately.
What technology is used to detect tuberculosis cases?
Negussie Beyene: The standard method used in most laboratories is still microscopy, a technique that is over 150 years old and has limited effectiveness, detecting only 30 to 40% of actual cases. That’s why we reanalyze microscopy-tested samples using more sensitive methods. Our innovative approach relies on specially trained rats, which are trained in Tanzania to identify tuberculosis by sniffing sputum samples. When a rat signals a potentially positive sample, we confirm the diagnosis using a cutting-edge molecular technique called “Xpert Ultra.”
Aline Serin: Using rats offers two major benefits. First, they can rapidly detect positive samples, enabling early patient care. Second, by using them as a pre-screening method, we drastically reduce screening costs by limiting the use of molecular identification cartridges, which are extremely expensive.

What have been the biggest challenges faced in the AHRI-APOPO project?
Negussie Beyene: One of the biggest challenges is undoubtedly population mobility. This issue has been exacerbated by the Corridor Project, which is relocating communities and dismantling some health centers. As a result, some patients move to other areas before we can deliver their screening results. To address this, we try to track them down by sharing their names with regional coordinators of the National Tuberculosis Control Program, so they can locate these individuals and ensure they start treatment. Together with the city’s health authorities, we are also working on mapping the relocation patterns of these urban populations to improve follow-up care.
What are the project’s results so far?
Negussie Beyene: The project has been well received and is progressing according to our objectives. To date, we have reached six urban areas, and we hope to reach all 11 urban areas and 49 districts of Addis Ababa by 2026. By reaching people directly where they live, we have detected 173 tuberculosis cases. Through our secondary screening strategy, we identified an additional 752 cases. This is important, because an untreated person can infect 10 to 15 other people per year. Overall, our program has helped raise awareness among more than 140,000 people about tuberculosis.
Aline Serin: We would not have been able to roll out this innovative project without the support of L’Initiative, both financial—nearly €2 million were invested—and technical. This support has allowed us to test strategies that do not necessarily fit within the framework of the Global Fund, helping us explore new, effective approaches to TB screening and treatment.